Signal and Image Processing: Making Models to Serve Health
The Signal and Image Processing Laboratory (LTSI) celebrated its 50th anniversary last November. Intended for military applications when it launched in 1969, this Inserm/Université de Rennes 1 Joint Research Unit now devotes itself entirely to the application of digital sciences to health.
« We provide doctors with interpretation and decision-support tools to improve the treatment of certain diseases », explains Lot Senhadji, director of the Signal and Image Processing Laboratory (LTSI)* in Rennes. These include epilepsy, heart failure, sleep apnea, cardiovascular disease, and cancer.
Research at LTSI starts with « signals » – observable parameters in patients that characterize cardiovascular system function, or brain function in the event of epileptic seizures... In order to improve their understanding of these functions, the researchers issue hypotheses on the mechanisms underlying these signals, which they then model. They reproduce, in a way, biological processes in silico, such as the network of blood vessels – and their deformation and elasticity in the case of the cardiovascular system – thanks to powerful software applications. Doing so determines whether their initial hypothesis is correct: should the model produce results similar to what happens in reality, then the predicted mechanisms are indeed those at work in reality!
Thanks to this approach, the LTSI researchers can, for example, plan a cardiovascular procedure by modeling the various surgical strategies and by selecting the most pertinent, in a virtual setting. They can also aid the treatment of epileptic seizures by enabling identification of the brain regions from which they emerge. Finally, they can develop medical devices, such as electromechanical stimulators that are able to treat arrythmia or stop sleep apnea.
The laboratory has produced a succession of innovations. Within the last 5 years it has filed 145 invention disclosures and 47 software applications. It manages 30 patent families and has very recently been associated with the creation of a startup.
Here we visit a laboratory in which engineers and clinicians work side by side.
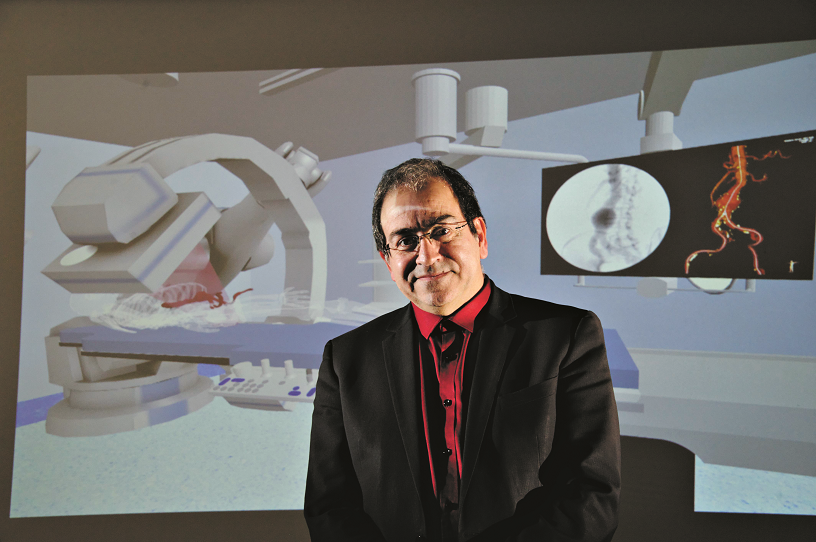
Lotfi Senhadji is the director of the LTSI, which brings together 160 research players, 60% of whom engineers and 40% hospital practitioners. Its teams are transdisciplinary in nature:
- Sesame, dedicated to severe epilepsy
- Sepia, specialized in cardiorespiratory diseases of the adult and preterm neonate
- Impact, dedicated to assisting cardiovascular operations and radiotherapy
- Metriq, dedicated to measuring parameters accessible by imaging
- Medicis, dedicated to surgical decision-support
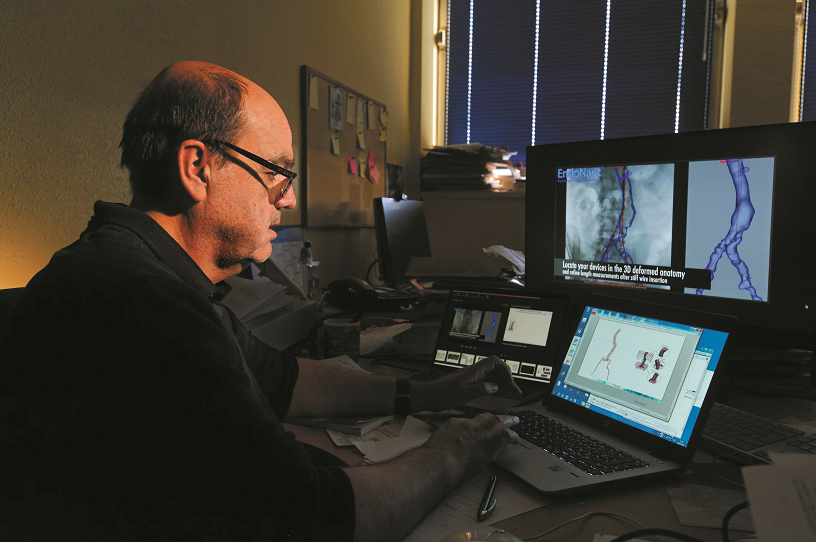
On the computer screen above, an artery shows an aneurysm – an abnormal dilation of its diameter. In anticipation of a minimally invasive procedure and based on pre-operative images taken from the patient, Impact team co-leader Pascal Haigron models the ideal pathway to use to guide the prosthesis to the damaged vessel. This tool also ensures that the patient is capable of undergoing such a procedure: tortuous or calcified arteries would make it too dangerous, in which case the doctors would opt for surgery.

Alfredo Hernandez, leader of the Sepia team, holds in his right hand the prototype of a medical device called Pasithea which is used to detect and stop sleep apnea, and in his left its miniaturized version. Thanks to this system, 75% of the patients monitored in the Hypnos study saw the duration of their apneas decrease significantly.
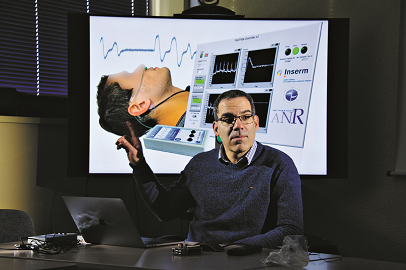
The scientist presents the three elements that make up the Pasithea system, which are capable of wireless communication: a system for recording cardiac and respiratory signals that detects the onset of apnea (nasal cannula and on-screen electrocardiogram), a mechanical stimulation system placed behind the ear, and an application to process the various signals in real time and emit stimulation that is appropriate to the patient.

Pacemakers are implantable devices that supply electrical pulses to stimulate the cardiac muscles when the heart beats too slowly or stops beating altogether. In order to develop new-generation implants, scientists are studying the various data recorded by the sensors in order to detect abnormalities that warn of a dysfunction — information which, once incorporated in the software of an implant, will enable it to anticipate the occurrence of serious events and prepare personalized therapy.

Doctoral student and Sepia team member Quentin Gillardin is developing the prototype of a device that stimulates the vagus nerve, thereby slowing the heart. Some patients present overexcitation of this mechanism and therefore blocking the overflow of information that circulates between the brain and the heart could enable the development of new functions for incorporation in future cardiac stimulators.

Fabrice Wendling, leader of the Sesame team, is interested in the biomarkers that make it possible to identify the networks linked to the onset of epileptic seizures, which differ according to each patient. Localizing them is crucial for those whose seizures do not respond to medication (30% of patients) and in whom surgery could be envisaged in order to remove the epileptogenic networks.
The epileptogenic networks are identified by stereoelectroencephalography (SEEG), which involves inserting very fine electrodes into the brain in order to record its electrical activity and identify the regions in which this activity is abnormal. Next up for the Sesame team is the Execom project, which will involve the development of a software application capable of identifying these epileptogenic regions more easily based on three new biomarkers obtained via SEEG.
Note:
* unit 1099 Inserm / Université de Rennes 1
